Although I shut down back in 2017, I am opening this blog to once again share my story with the hope that it may resonate with someone.
Since then, I’ve gone through several more operations and treatments. From each treatment, surgery, and medication, there are been impacts to my body, mind, and soul which fractures a sense of self. It’s traumatic each time. Even though I may be the one making the choice with my team, my body does not.
Through resilience, I can give myself grace, patience, and healing over time. We can adapt with what we’re given. And for me, I’m leaning deeper into the suffering to learn from life through the lens of my curiosity when I can. There are limitations, walls, and barriers. Some may had been created for me to survive but now need to be broken as they are no longer helpful. The idea is to bridge the gaps between control and the unknown. I need to ground myself with what I do know and surrender from what I do not know: objective vs subjective.
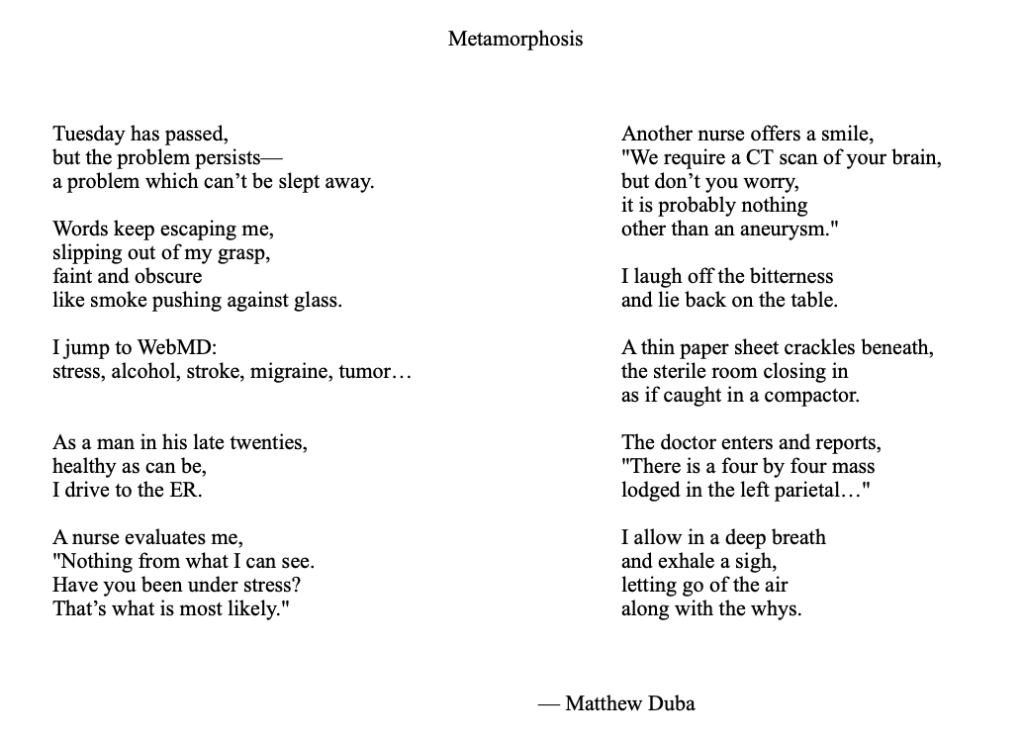
I had a brain hemorrhage on 2020 right around the pandemic which shattered me. I had no control with what happened. On that day, I was experiencing another focal seizure: tingling, numbness, fatigue, and worsened expressive aphasia. I could feel that something new and worse was happening but couldn’t pinpoint it. I had to call out to get to Lauren and lied down to rest but new that I needed further help. I fell into a fog, and she called for an ambulance to rush me to a hospital.
When I made it to the hospital, I was in and out of a daze while they were asking me questions. I couldn’t follow what was happening and passed out again. After waking up, I learned that I had consciousness but had no control and no memory for the day.
The neurosurgeon stopped the bleeding, discovered the tumor, and chose to cut out the tumor. He saved my life. I had a speedy recovery with the help of occupational and physical therapy. I was able to get back home soon after.
However, he also did not send the tumor to pathology and did not give the same care that I was given from my main team. I had worsening headaches. I could almost feel the screws along my scalp and would sometimes soothe my head by massaging the tenderness. There was something wrong while comparing from my first surgery. I knew that I would need another surgery to fix my head.
Along with that, I lost vision on the right side with both eyes. I won’t get that back. And with my speech, I wonder if the neurosurgeon cut too deep or caused a worsening impact with my language. On top of that, I was given wrong information with my insurance. I kept asking to make sure that my speech therapy was covered at home. I wanted to trust them. But I had a feeling that I was missing something. I was given a bill much later after processing the insurance and had to pay out of pocket because several sessions were not covered. I felt like I had an awful experience while also trying to grapple and understand what happened to me.
Despite feeling a loss of control and anger, the fact is that they did their best to save and help me while I somehow needed to cope from traumas and navigate which directions to go next.
Soon after, I had a recurrence within the year and got back on Temodar. Then there was enough time to recover from the surgery to have another which aligned for me to have GammaTile. I was the first patient in UT Southwestern, and the experience was incredible. Love comes through this medical center. Although I already felt fortunate to have their care, the appreciation is magnified.
Afterwards, I coordinate my team locally with Highlands Oncology Group where similarly they deeply care for the patients and have given emotional and guidance. They follow-up with me with MRI and have helped to have infusions to resolve swelling from the impacts of the radiation (necrosis).
I have to coordinate between two teams, and this is just a touch of how complicated healthcare can be for a patient to navigate their healing.
Now I am finished a treatment for the necrosis, and I’m in the middle of chemotherapy (lomustine and procarbazine) from a recurrence this year. And I’m freaking tired of feeling like I have to wait to recover. That’s me. I’m tired of doing that, but it is a lot harder. It’s pushing against the grain which is beyond uncomfortable. There is this strange space between this chemotherapy and continuing to recover from my brain hemorrhage. This is where I’m leaning deeper into the suffering along with all these techniques and practices that I’ve learned along the way. I simply have to follow through by learning to trust myself again. A deep layer involves this inner confusion while lose a sense of self. I need to find that again.
So, here I am. Back to this space with my blog. I need to open up again, and I’ve been given gentle nudges from the support of several others where I am deeply grateful. Time to be true to oneself and yield to the gravity from the traumas. All we can do is our best.